Eswatini on Tuesday became the first country in Africa to receive lenacapavir, a twice-yearly HIV prevention injection that global health experts say could transform efforts to curb the virus across the continent.
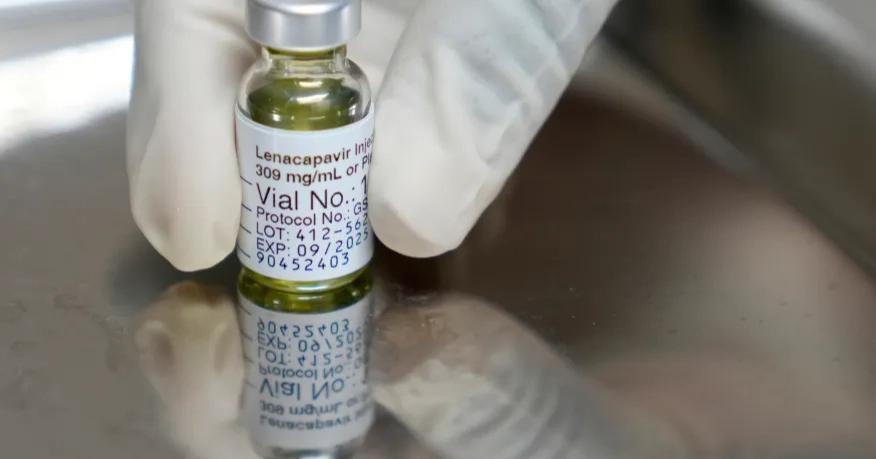
The drug — developed by Gilead Sciences — has shown near-complete protection in trials. Its initial rollout is part of PEPFAR’s partnership with the Global Fund and will eventually expand to 10 high-risk African nations, aiming to reach at least 2 million people by 2027.
Gilead CEO Daniel O’Day called the launch “extraordinary,” noting it marks the first time a new HIV medicine has reached a sub-Saharan African nation in the same year it was authorized in the United States. The U.S. approved the injection in June.
Although the U.S. foreign aid budget has been sharply reduced under President Donald Trump — affecting key health programs in Africa — officials said demand prompted an increase in the number of doses distributed this year from 250,000 to 325,000. Zambia also received its first shipment Tuesday, and Gilead is seeking regulatory approval in Botswana, Kenya, Malawi, Namibia, Rwanda, Tanzania, Uganda and Zimbabwe.
Across Africa, more than 25 million people are living with HIV. In Eswatini — a nation of 1.2 million with the world’s highest infection rate — about 6,000 people are expected to receive the injection initially, with a focus on preventing transmission from mothers to newborns. Over 200,000 people in the country currently live with HIV, most supported through PEPFAR programs.
The rollout comes as Eswatini, the continent’s last absolute monarchy, faces criticism over human rights concerns and its participation in the U.S. third-country deportation program.
The World Health Organization cleared lenacapavir for use in July, and UNAIDS has described long-acting injectables as a vital new tool at a time when funding cuts could jeopardize progress. South Africa’s health minister, Aaron Motsoaledi, praised the drug as “groundbreaking” but warned that limited supplies could complicate its national rollout planned for April 2026. He also welcomed Gilead’s decision to slash the price from more than $28,000 per patient annually in the U.S. to about $40 for lower-income countries.
Still, the launch has revived long-running disputes over access and manufacturing. South African civil society groups have criticized Gilead for withholding voluntary licenses from local producers, despite the country’s role in key clinical trials.